Pinched Nerve in Hip Relief Guide (No Doctor Visit)

As a clinician and coach who’s spent 12+ years poking at cranky hips and calming down nervous systems, here’s the fast truth: a pinched nerve in hip pain-land usually means nerve compression from your back, hip, or tight tissue. It can feel like burning, tingling, numbness, or a zinger down the leg. Think sciatica, meralgia paresthetica, groin pain, or that awful “electric” shock that makes you freeze mid-step. I’ve seen it in runners, lifters, desk workers, me included. Not glamorous. Very fixable.
What it actually feels like (no drama, just facts)
In my experience, nerve pain has a vibe. It’s not dull. It’s sharp or buzzing. It may shoot to the thigh, knee, or even the foot. Sometimes just the outer thigh burns. Sometimes your hip feels stuck and your foot goes numb. Good times.
Quick checklist you can scan
- Burning or tingling: on the outer thigh? Could be the lateral femoral cutaneous nerve (that’s meralgia paresthetica).
- Pain from low back to butt to calf: Classic sciatica pattern.
- Hip flexor tight, groin ache, numb front thigh: Maybe femoral nerve irritation.
- Pain worse when sitting relief when lying flat: Often nerve compression hates flexion.
- Weak ankle or foot drop: That’s a red flag; call a pro now.
If you want a straight medical summary, the MedlinePlus overview of pinched nerves has a clean, simple explainer. I send patients there when they want the short science version.
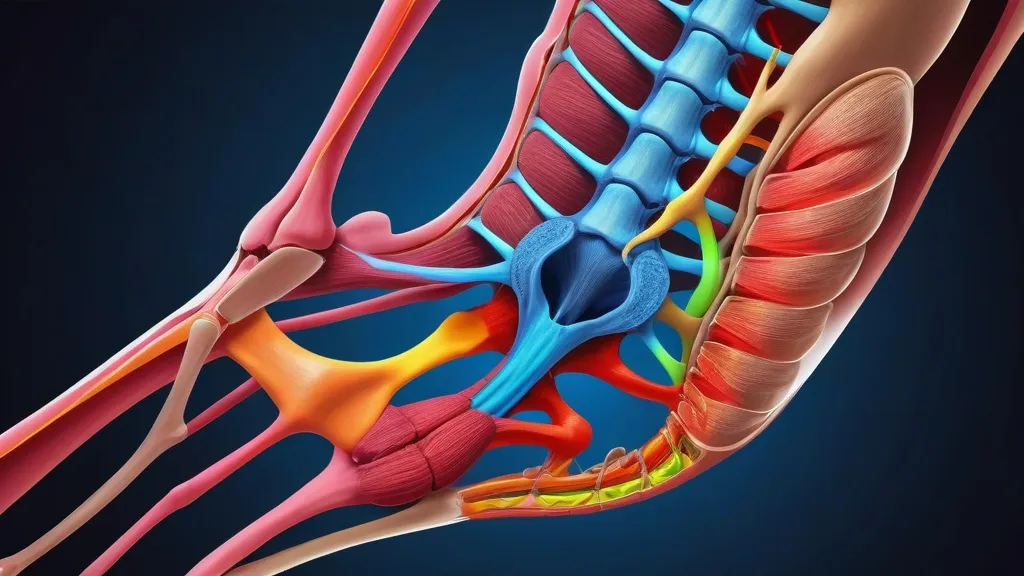
Why nerves get grumpy in the hip zone
I wish I could tell you there’s one cause. There isn’t. Here’s the big five I see weekly.
- Lumbar disc irritation: a herniated disc can inflame nerves that feed the hip and leg (lumbar radiculopathy).
- Piriformis syndrome: the tiny butt muscle hugs the sciatic nerve; too tight, and it complains.
- Meralgia paresthetica: the lateral femoral cutaneous nerve gets squashed under tight belts or a cranky pelvis.
- Hip impingement + weak glutes: jammed joint + poor control = extra pressure on nearby nerves.
- Too much sitting: hips flexed all day, nerves on stretch, tissues stiff. Desk chair villain arc.
For deep-dive nerding (I say that with love), the NINDS guide on sciatica lays out how nerve roots in your spine spark leg pain. It’s not always “the hip.” Sometimes it’s the back wearing a hip mask.
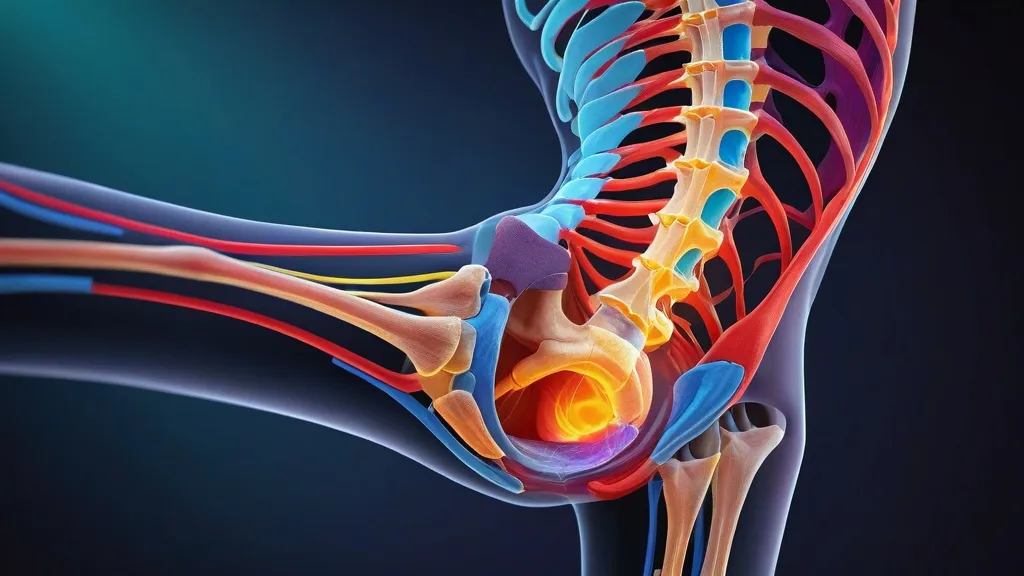
Sciatica vs. Meralgia Paresthetica vs. Femoral Nerve: who’s who
I’ve always found side-by-sides help people get it fast. Here’s a simple comparison I use in clinic.
| Nerve problem | Where it hurts/feels weird | What makes it worse | What often helps |
|---|---|---|---|
| Sciatica (sciatic nerve) | Back/butt down back of thigh, calf; tingling or zaps | Long sitting, bending, coughing | Walking, gentle extensions, glute/hamstring mobility |
| Meralgia paresthetica (LFCN) | Outer/front thigh burning, numb patch | Tight waistbands, belts, heavy tool belts | Looser clothes, hip flexor mobility, core control |
| Femoral nerve irritation | Front thigh, groin; maybe quad weakness | Deep hip flexion, long sitting | Prone props, quad/hip flexor release, gentle nerve glides |
DIY tests (the no-equipment kind)
- Walk test: if walking eases symptoms in 5 to 10 minutes, you may have flexion-intolerant nerves (back extension often helps).
- Chair swap: sit on a firm seat, hips a bit higher than knees. Better? Compression from deep flexion was part of it.
- Belt experiment: loosen the waistband. If outer thigh burning fades, suspect meralgia paresthetica.
- Slump test (gentle): sit tall, then slouch and straighten the knee. If tingling ramps, nerves are sensitive today. Don’t force it.
What actually helps (the short list I give friends)
- Motion over medication: walk 5 to 10 minutes, 3 to 6 times a day. Keep the pace easy.
- Positions of relief: if lying face down on elbows helps, do that for 1 to 2 minutes, a few times daily.
- Unload pressure: swap tight pants/belts, change chairs, add a footrest, stand more.
- Chill then warm: 10 minutes of ice for hot, angry pain. Then later, heat for stiff muscles. Alternate as needed.
- Anti-inflammatory basics: sleep, water, protein, short walks. Not sexy. Very effective.
I write a lot about the boring-but-crucial stuff like warm-ups, smart progressions, and deloads here: injury prevention. It’s the unglamorous path that keeps you training.
A simple 7-day plan I actually use
- Days 1 to 2: easy walking, gentle back extensions if they help, zero deep stretching.
- Days 3 to 4: add light glute bridges, side-lying clams, and hip hinges with a broomstick.
- Days 5 to 7: short circuits, hinge, carry, step-up. Stop before the nerve gets spicy.
If you’re also rehabbing a cranky knee (because of course the knee got jealous), I’ve got a field-tested knee injury rehab plan that pairs well with hip nerve work. Keep the whole chain happy.
Nerve glides that don’t make you swear
People love to overdo nerve flossing. Don’t. Nerves like calm movement, not aggressive tug-of-war.
- Sciatic slider: sit tall, straighten the knee as you look up; bend the knee as you nod down. 8 to 10 easy reps.
- Femoral slider: lying on your side, pull your heel toward your butt a little as you look up; release as you look down. 8 to 10 reps.
- LFCN kindness: gentle hip flexor stretches, pelvic tilts, and changing waistband pressure. No hard tugs.
If you’re an athlete who gets lost in accessory work, I keep a curated section on fitness for athletes so you can stop guessing and start building resilience.
Ergonomics that actually matter
- Hips a touch higher than knees when sitting.
- Feet flat, weight not stuck on one side.
- Stand every 30 to 45 minutes. One lap around the room.
- Sleep with a pillow between knees (side) or under knees (back).
When it’s not “just the hip”
I’ve seen folks chase hip stretches for months when the real issue was the low back. If pain shoots below the knee, or you’ve got numbness plus clear weakness, the source is often the spine. That doesn’t mean doom. It means targeted work and, sometimes, imaging if red flags show up (severe weakness, bladder/bowel changes, fever, trauma).
If your sport keeps gifting you flare-ups, this breakdown of injuries by sport is eye-opening. The patterns are predictable, which means preventable.
Common traps I still see (and yes, I’ve done them)
- Over-stretching the hamstrings: when the nerve is already irritated. Instant regret.
- Hammering core crunches: that crank the spine into flexion for 20 minutes. Your nerve hates you now.
- Max deadlifts “to test it”: Please don’t test fire alarms with actual fire.
- Ignoring belts, tight pants, and heavy tool belts: Pressure is pressure.
And hey, sometimes the biggest limiter is fear. Pain is loud; the brain gets jumpy. I write a lot about reframing pain and building confidence here: sports psychology. It matters more than you think.
How I coach a return to lifting and running
- Volume before intensity: more easy sets, less heavy load.
- Neutral-ish spine on hinges and squats. Your hip will thank you.
- Short strides for runners, high cadence. Ease the hip flexor load.
- Finish with a walk, not a deep stretch. Cooling nerves like movement, not static holds.
One more note on labels
People obsess over the name. Is it sciatica? Is it femoral? Is it meralgia paresthetica? Labels help guide, but your plan is mostly the same: calm the nerve, remove pressure, build strength, return load in steps. If you want a tidy primer on the thigh-burning one, the Wikipedia entry on meralgia paresthetica is actually decent for quick context.
My go-to progression (so you don’t overthink it)
- Phase 1: find positions of relief, walk, breathe, and sleep more.
- Phase 2: gentle nerve sliders, easy glute and core work.
- Phase 3: hinge/squat patterns with light load, carries, step-ups.
- Phase 4: return to sport with intervals and rest days.
Cheat-sheet table
| Do | Don’t | Why |
|---|---|---|
| Walk in short bouts | Sit for hours | Motion reduces nerve sensitivity |
| Use positions that ease symptoms | Push through zinging pain | Calm nerve first, then load |
| Build glute/core strength | Chase only stretches | Strength protects joints and nerves |
| Change belts/chairs/posture | Ignore external pressure | Less compression = less irritation |
If you’ve been told your pinched nerve in hip area means “no lifting ever,” I disagree. Most of my clients return to full training. We just stack the steps and stop pretending pain equals damage every time. Boring, methodical, effective.
And yeah, I still get flare-ups if I sit too long on flights. I move. I breathe. I do three sets of bridges and some sciatic sliders. Then I go lift. You can do this too. Slowly, then suddenly it’s better.
FAQs
-
How do I know if it’s sciatica or just a tight muscle?
If pain shoots down the leg with tingling or numbness, and sitting makes it worse, think sciatica. A tight muscle feels more local and dull.
-
Will stretching my hamstrings fix this?
Early on, probably not. Gentle nerve glides beat hard hamstring stretches when nerves are irritable.
-
Do I need an MRI right away?
Usually no. Unless you have red flags like severe weakness, bladder/bowel changes, fever, or trauma, try 2 to 6 weeks of smart care first.
-
Can I still work out?
Yes, modify. Easy walks, light hinges, glute work, and stop before symptoms spike. Load returns in steps.
-
Why does my outer thigh burn when I wear tight jeans?
That screams meralgia paresthetica, pressure on the lateral femoral cutaneous nerve. Loosen the waistband and work on hip flexor mobility.
Anyway, that’s my rant-meets-guide. If this helps you take one calm walk and skip one panic stretch, I’ll call it a win.

I’m Benjamin Clark, dedicated to elevating your athletic performance. Get targeted fitness plans, injury prevention techniques, sports psychology insights, and the latest in nutrition. Let’s train smarter.




How can I differentiate between sciatica and meralgia paresthetica based on symptoms?